As healthcare organizations experience various economic hardships, strategic facilities planning can improve financial capacity and value. At present, many hospital and health system leaders view the purchase and maintenance of facilities as a necessary business operations expense. And a growing expense at that.
Of 200 healthcare facilities professionals surveyed, 38% are increasing their budgets for new hospital construction in 2023, according to a recent survey conducted by the Health Facilities Management magazine. Additionally, 26% of survey respondents say their projects are over budget and behind schedule — up from 20% last year and the highest level in over a decade. But when healthcare facilities planning is approached strategically, facilities can positively impact organizations by enabling cost savings and enhancing value to communities and employees. For example, a smartly planned and maintained healthcare facility is more likely to enable efficient workflows and positive patient experiences. This leads to lower spending through improved efficiency, reduced employee turnover and even shorter length of stay for patients.
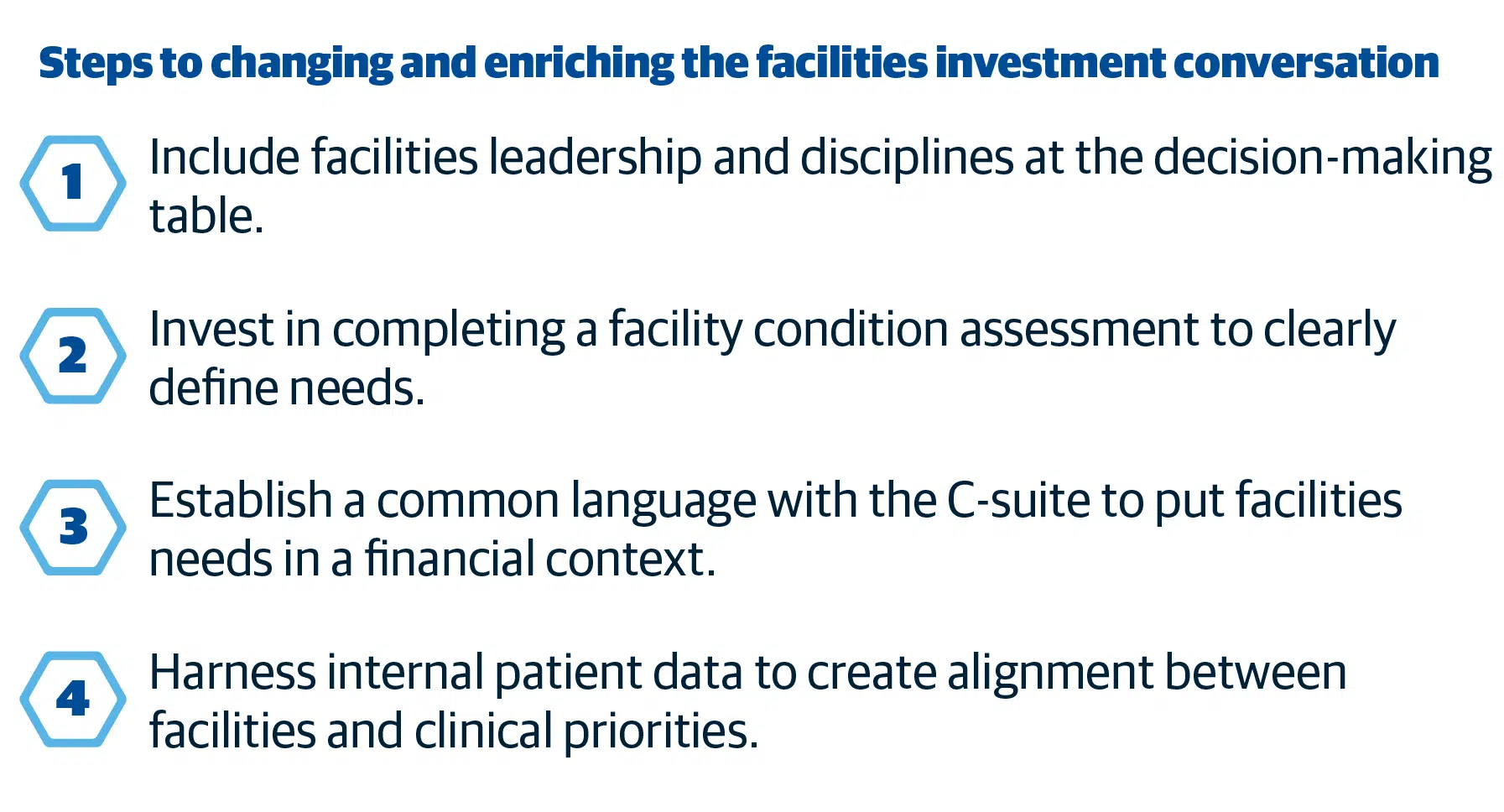
Here are four steps savvy facilities, finance and operational leaders can adopt a deliberate approach to healthcare facilities planning.
Step 1. Include facilities planners at the decision-making table:
The executive team at most health systems and hospitals doesn’t include leadership from the facilities planning team. Instead, facilities planners usually report to the COO or the CFO, who in turn relays facilities plans and investments to the rest of the C-suite and Board members.
This is an inefficient way to communicate investment needs and priorities because CFOs and COOs generally aren’t well-versed in the complexities involved in facilities planning. Although qualified financial and operational administrators, these leaders have less experience articulating the need for certain facilities investments or understanding the rationale for making particular design decisions before embarking on expensive construction projects.
By including a facilities planning leader in the C-suite, healthcare organizations are better positioned to make decisions suited to their unique needs and challenges, boosting overall long-term financial health.
Step 2. Conduct a facility condition assessment:
Facilities planning and maintenance are highly complex endeavors for most healthcare organizations due to the complicated nature of providing healthcare services and the vastness of most provider networks. A continuous cycle of improvements and new construction projects are required to not only provide lifesaving services but to remain competitive in the marketplace.
A best practice to guarantee your healthcare organization makes facilities planning decisions that drive short- and long-term value is to conduct facility condition assessments. A facility condition assessment (FCA) is a technical assessment measuring the condition and functionality of all the assets in an organization’s facilities portfolio. The result is a verified, accurate and reliable inventory of an organization’s facilities infrastructure, including all physical assets that require funding to maintain. An FCA will also codify the current condition of the building including interiors and other aspects of the built environment. By performing an FCA, organizational leaders put themselves in a better position to assemble and articulate facilities needs, prioritize investment options and ensure a defined strategy is behind every decision.
Hospital and health system leaders might be wary of the investment it takes to complete FCAs, but the benefits of doing so greatly outweigh the cost. Completing an FCA allows healthcare organizations to make informed investment decisions and attain immense savings, which is imperative as they face rising costs and slim operating margins.
Discover how hospitals like yours are implementing winning facilities investment strategies.
Step 3. Establish a common vocabulary:
Once facilities planners secure a seat at the tables of top leadership, they must know how to communicate priorities effectively.
Facilities planners must be able to speak the language of the people in the C-suite and in the boardroom. They should avoid using jargon or sharing unnecessary details. Ideas won’t resonate with the C-suite or the Board if the conversation focuses solely on what needs to be fixed, or how much it will cost. As leaders manage tight budgets, they’re increasingly likely to select investments directly impacting patient care. Recognizing this focus, planners must connect facilities projects and improvements to their organization’s mission and strategic vision.
Instead of saying, “The boiler is broken, we need cash to fix it,” speak to the implications it will have for patients. Then, you begin to move to a place where you’re engaging in a shared problem and a shared solution, not a competition over resources.
Step 4. Augment FCA findings by harnessing data:
In determining facilities planning needs, healthcare leaders should use internal data sources including HIPPA-scrubbed patient data from the Electronic Health Record. Patient data can offer valuable insights into throughput, length of stay and admissions for each medical unit, which are immensely helpful data points for facilities planning.
Despite the widespread adoption of Electronic Health Records, the healthcare industry overall has been slow to use this kind of data to make strategic facilities decisions. If your organization has invested in an FCA, and you can begin to use your other data resources to improve and inform that information, you’ll be on a much better track to success.
A conversation about risk
By embracing the key principles outlined above, healthcare organizations can realize benefits from facilities planning rather than viewing it only as a necessary expense. For example, after implementing strategic facilities planning measures, healthcare leaders might gain a new perspective on deferred maintenance. Often seen as a daunting, costly issue for large institutions, deferred maintenance should instead be viewed through a risk management prism; not all deferred maintenance needs to be resolved.
There’s a lot of deferred maintenance that can run to fail without becoming a critical expense or impacting operations. By implementing strategic facilities planning, healthcare organizations can arm themselves with the critical support and information necessary to understand which deferred maintenance items should be prioritized, thereby improving overall financial capacity and mitigating unnecessary risk.
See how Gordian can help you in every phase of the building lifecycle.
How Gordian Can Help You Reframe the Conversation on Facilities Value
As hospitals and health systems reevaluate expenses such as facilities planning, it’s essential to have a partner. Gordian works alongside healthcare organizations to create relevant and strategic facilities planning programs, providing tools and support for facility managers and financial leaders to achieve leadership buy-in. We also help organizations gather and evaluate data sources pertinent to their facility planning goals.